AnalyticsMD, which is launching out of Y Combinator‘s latest batch, is a startup tackling a difficult but very worthwhile problem: how to boost the operational efficiency of hospitals and improve patient care by helping staff make better choices about how resources are allocated. Its founders liken their product to an “air traffic controller for the hospital and healthcare system”.
Their real-time analytics platform predicts changes in demand so that resources such as extra staff and beds can be brought in before they are needed to prevent scenarios such as emergency room waiting times spiraling outside target limits or the quality of patient care suffering. The HIPAA compliant SaaS software has been rolled out to several paying customers in the U.S. healthcare sector so far, including a major San Francisco Bay Area hospital system.
The key to understanding AnalyticsMD’s proposition is the large-scale, machine learning prediction engine at the core of their platform, say co-founders Brent Newhouse and Mudit Garg. This ingests “a spectrum” of real-time data signals — from electronic medical records, to staffing systems and outpatient numbers, along with granular on-the-ground signals such as bed sensors and emergency call button data, to external factors gleaned by scraping public data such as weather info, disease seasonality and even local events which might have an impact on hospital admissions — looking for patterns to generate its demand predictions.
Predicting accidents that end up in the ER does sound a tad oxymoronic but that’s exactly the point of such complex, multi-signal AI-powered analytics platforms. The basic concept being: feed the machine enough data and the learning algorithms will find the patterns, or at least be able to predict likelihoods with decent accuracy. So that’s what AnalyticsMD says its platform can do — and with a high degree of accuracy. (In testing of its algorithms it says it has measured measured “mid-step accuracy” in the 90% range of predicting volume a day ahead, or predicting census of a unit a day ahead, although Garg stresses it’s not putting those test figures in front of customers.)
The software weighs up demand probabilities and considers the various costs involved, meaning financial costs such as staffing and beds but also care costs, so crucial factors such as quality of service and patient satisfaction, before generating its real-time resource recommendations via a decision layer — known as DecisionOS.
“There’s always an element of the unknown [when generating predictions] but that’s why the final layer that we tack on top of the prediction engine is this decision layer. What it’s doing is it’s saying ‘I know historically when I have predicted this is how off I am, and based on that I know what is the cost of being off and what is the benefit of that, and let me optimize my answer based off of that’,” says Garg.
“It’s a concept borrowed from industrial engineering which is if you think of the prediction not just as saying we think there’s going to be exactly 23 patients, not more no less, but instead think of it more as a distribution of predictions… we know roughly what the probabilities of being off by a little bit here, a little bit there are, based on how this algorithm has performed in the past. If you have a sense of what that distribution looks like you can make your decision based on [the relative costs],” adds Newhouse.
“If we know historically what the distribution on those predictions looks like you can actually optimize and minimize those costs and pick a decision — even if you don’t know the exact number of patients, you can make a decision that balances the trade off of being too conservative or not conservative enough based on those costs.”
More than a dashboard
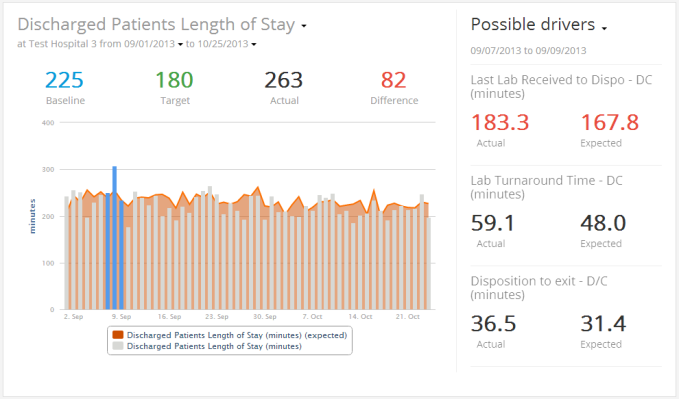
This predictive core — they argue — sets the product apart from rival software products which just plug multiple data signals into a dashboard view for hospital staff to interpret themselves. The problem with the dashboard approach in healthcare operations is staff simply don’t have time to be triaging all this data themselves. And while AnalyticsMD does offer its own real-time dashboard view too, its added layer of data processing helps hospitals achieve greater operational efficiencies by providing a nudge ahead of time.
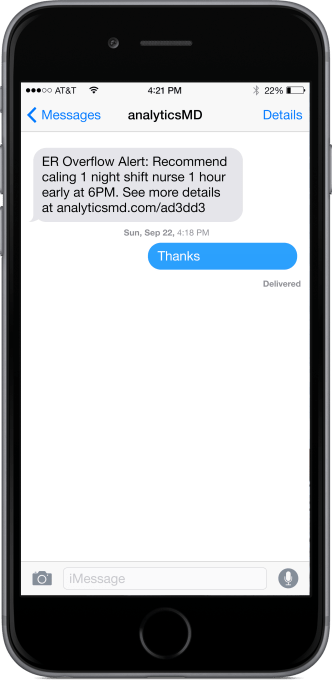
Recommendations generated by DecisionOS are delivered to hospital staff as pre-emptive alerts, perhaps sent as a mobile text message (as in the below example) or via a phone call to their device. Whatever device and medium is most appropriate for reaching that particular healthcare providers’ staff.
“These users are ones that are constantly battling fires that are happening in the hospital and taking care of patients, so to expect them to continuously check a dashboard, make sense of what’s going on, see if it’s causing a problem and happen to see it at the right time and then decide what’s the best data-driven decision, based on that, is really hard,” says Garg.
“We started with [a real-time dashboard] at first… and realized that, and then built a whole bunch of statistical intelligence to do; first: automatic detect if there is anything unusual happening and let the hospital know; second: find the root causes, we actually filed some IP on that, to statistically find the root causes, so if an emergency room is backing up is it because we had a lot of patients, is it because they were sick, is it because labs didn’t work fast enough, what were the real root causes; and then [DecisionOS] predicts, based on what it’s seeing — we see 10 patients now in the waiting room, it’s going to get to 20, to prevent this you need to call a doctor in one hour earlier, or you need to open that bed. And that’s been really, really amazing for our customers.”
The initial application targets for AnalyticsMD’s tech are emergency departments, operating rooms and outpatient capacity. But the team sees scope to expand to fit all sorts of care and clinical operational facilities and needs over time.
Indeed, the platform’s recommendations can and are already being tailored to highly granular, predictive care scenarios — such as helping to reduce the number of patient falls. Or even to detect which patients may not have had the best service in the hospital.
The team claims one early implementation of its platform was able to cut the number of patient falls in half over a 1.5 month period, based on analyzing a combination of data signals such as when a patient presses a call button for help, how long it takes a nurse to respond, what the patient was asking for, how much they were moving around in their bed and so on.
“Historically we detected patterns to patients that had fallen and used that combination to be able to say who are the patients who are likely to fall.
“We do use a whole bunch of machine learning algorithms that help take out any unknowns in the equation,” adds Garg.
Another compelling benefit Newhouse points to of having an analytics platform helping to manage hospital operations, rather than just a dashboard — or even a dedicated human team focused on optimizing operational efficiency — is that it provides unbroken continuity between staff changes. So, for instance, a nurse just arriving for a day shift will be automatically in the loop about any ongoing issues from the night before — because the platform provides the data overlap as human staff come and go.
But what about the other humans in this equation — the patients? Are they aware of how the things that they do and that happen to them in hospital are now being processed, and how certain actions might trigger certain healthcare outcomes? In its current rollouts Garg says is only utilizing data elements that hospitals were already capturing, so patients have not been explicitly made aware of this additional, more joined-up layer of data-processing going on around them.
“I think the patient’s experience right now is probably one of pleasant surprise when the hospital walks in and says ‘we noticed you may not have got the best service, what can we do to help?’. They probably just see the hospital as being a lot more responsive. Without necessarily seeing the tech explicitly,” he adds.
However he does go on to specify that if a hospital started asking for additional decisions that maybe required additional data elements to be captured then the team would “definitely want to have a conversation with the patients to make sure they are comfortable with that”.
Newhouse also points out that AnalyticsMD makes a point of not capturing personal data such as patients’ names or dates of birth. “That was a very conscious decision we made. From an operations perspective that information isn’t really needed and why take it if we don’t need it?”
The original concept for AnalyticsMD dates back some four or five years, according to Garg, after he and Newhouse (who both have engineering backgrounds) met while working in hospitals on operational issues — where they saw how day to day operational challenges and inefficiencies could impact front-line care. The team’s third co-founder, Ian Christopher, brings the algorithmic expertise — having worked on predictive software while at Stanford. A first version of their product was launched two years ago, followed by an MVP of the current iteration some six months ago, and the latest version, with the DecisionOS layer, landed in December.
The startup has raised $720,000 in seed funding so far, with investors including YC and some undisclosed U.S. angels. Given it’s taking revenue, it’s not in a position where it needs to raise more funding at this point but the co-founders speculate that if they convert all the interest they are seeing into paying customers they may look to bring on additional investors to help scale to meet demand.
In terms of their next steps, as they graduate from the YC program, they are focusing on the newly launched DecisionOS feature — including getting it rolled out to more customers. “We are flushing out the delivery mechanism of the DecisionOS and launching it in a 30 hospital system, hopefully soon, in all their emergency rooms. And then a few customers on the operating room side. And then our plan going forward is to mature that DecisionOS… And take the partners that we have today, many of which are large systems, and expand into all their facilities,” says Garg.
He adds: “Our goal would be to be in fairly substantial number of facilities in one geography, at least where we can start proving what the gross facility benefits are — for example picking out flu trends before they happen, picking out new diseases as they’re coming to the area — so we can start helping different systems which have silos of data derive benefit from each other as well.”