Twelve years after a first patient was identified as cured of HIV, the virus that causes AIDS, a second patient undergoing similar treatment was diagnosed as in long-term remission, according to a New York Times report citing an article to be published tomorrow in the journal Nature.
The report means that a cure for the disease is possible, but several obstacles remain before it can be developed and applied broadly, according to scientists quoted by the Times.
The findings are set to be presented at the Conference on Retroviruses and Opportunistic Infections in Seattle on Tuesday.
The successful treatment involved bone marrow transplants that were given to patients infected with HIV. However, the transplants were meant to treat the patients’ cancer — not the virus.
Because of the risks and side-effects associated with bone marrow transplants, using the treatment broadly as a cure for HIV likely isn’t a possibility, and drugs are available to control the infection.
What scientists find promising is the potential to replace infected cells with immune cells modified to resist HIV.
Speaking to the Times, Dr. Annemarie Wensing, a virologist at the University Medical Center, Utrecht, in the Netherlands said, “This will inspire people that the cure is not a dream.”
Dr. Wensing co-led the team of European scientists that studied stem cell transplants to treat HIV infection.
Backed by the American AIDS research organization AMFAR, the IciStem organization is the second group of scientists to cure a patient.
Twelve years ago, at the same conference, a German doctor described using bone marrow treatments to cure a patient who was being treated for leukemia. The transplants also cured the patient of HIV.
After that initial success several doctors tried to replicate the results, with little to no success. Either patients died of cancer or the virus returned when they stopped taking their anti-retroviral medication.
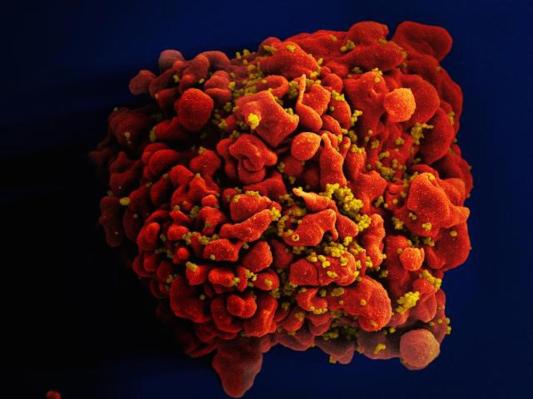
The crux of the treatment depends on using mutated immune cells that have a variant of the standard CCR5 protein. The mutation blocks HIV from infecting cells by stopping the virus from latching on to host white blood cells.
It’s a treatment that nearly killed the first patient it was used on. However, not all the conditions of that first cure apparently need to be replicated to ensure that a patient remains HIV-free following treatment.
The most recent patient was receiving treatment for Hodgkin’s lymphoma and as part of his therapy underwent a bone marrow transplant from a donor that had the CCR5 mutation to their cells. The patient took a course of immunosuppressive drugs as part of his treatment.
In 2017 the patient stopped taking anti-HIV drugs and has remained disease-free ever since.
Despite the success, there’s no guarantee that the new patient will remain disease-free. He’s undergone a series of tests to check whether the virus has returned, and, while all but one diagnostic revealed him to be HIV-free, doctors are still monitoring his situation closely.
This isn’t the first time that a scientist has identified the CCR5 protein as holding the potential for an HIV cure.
China’s now-disgraced and imprisoned scientist He Jiankui used gene editing to modify the DNA of two children so that they would have the mutated CCR5 — ostensibly making them resistant to the HIV virus.
While Dr. He’s research was premature, and was met with global condemnation, private companies and researchers are pursuing gene therapies to treat the HIV virus.
The Times notes that the CCR5 therapy that’s being developed is only effective on about half of patients who are infected with the virus that causes AIDS. Another half are vulnerable or infected to a form of the virus which uses a different protein to enter cells.
One important caveat to any such approach is that the patient would still be vulnerable to a form of HIV called X4, which employs a different protein, CXCR4, to enter cells.