More than ever, insurers and healthcare providers are looking for ways to reduce the cost of patient care. Wellth, which launched onstage today at TechCrunch Disrupt NY, thinks it solved one step of the puzzle.
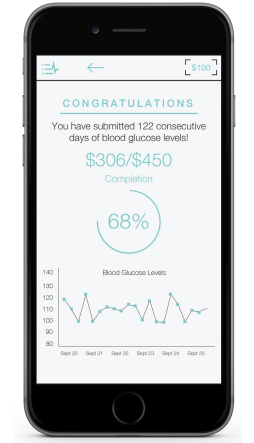
Many times, patients leaving a hospital will not follow the instructions given by caregivers, and the caregivers often don’t have the time to follow up with every patient. Using Wellth, patients keep track of their medical activities with the application, such as taking medication daily or registering their weight, and that information is shared with primary caregivers.
By doing that, Wellth can gather data about cases like diabetes and figure out what the best approach to constructing the best care patterns for individuals, CE nm x uzO Matt Loper said. Then, those individuals can be financially incentivized to follow those guidelines. It’s something that was partially inspired by Amazon’s recommendation model, he said.
 “Amazon has analyzed huge sets of data over the past 10 to 20 years and found patterns between different types of customers,” he said. “That’s exactly what we want to do in healthcare, look at huge sets of data and find patterns, and what is the optimal care for any specific person.”
“Amazon has analyzed huge sets of data over the past 10 to 20 years and found patterns between different types of customers,” he said. “That’s exactly what we want to do in healthcare, look at huge sets of data and find patterns, and what is the optimal care for any specific person.”
Getting hospitals to adopt the software is a challenge, but it’s an area that insurers are certainly interested in, if it reduces the cost of a person’s health care over the span of their lives. It also seems like something that private practices would be more likely to adopt. Many of the parameters are readily trackable, such as weight, taking medication, using an asthma inhaler and so on.
Around 30 percent of Medicare payments are under a new “fee for quality” guideline, which also incentivizes hospitals to ensure that patients are well taken care of and not just billing for procedures. That means that caregivers are incentivized to make sure that they aren’t getting readmitted due to not taking medication, or are catching major changes in their health before they become major problems. By next year, 50 percent of Medicare payments will be under those guidelines, and the goal is to be up to 70 percent by 2018, said Loper who, along with his co-founder Alec Zopf, has a background in biological and biomedical engineering.
Convincing the commercial side might be a bit of a different problem, but commercial institutions tend to follow changes in Medicare by a few years, Loper said. So far, the company hasn’t secured any major partnerships yet, but the most obvious first candidates would be organizations that are self-insured, like Google, or organizations that are a hospital and an insurance company, such as Kaiser Permanente.
“We can touch both sides of the equation and there’s a clear financial interest in taking care of patients,” Loper said.
The company raised a small friends and family round prior to launching.
[gallery ids="1153483,1153490,1153489,1153488,1153487,1153486,1153485,1153484"]